This video is available for licensing on our website. Click HERE!
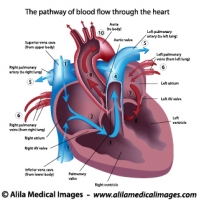
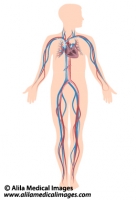
Venous return is the flow of blood from the periphery back to the heart’s right atrium. Venous return is important because the more blood returns to the heart, the more blood can be pumped out. In other words, venous return is the major determinant of cardiac output.
Venous return is achieved by several mechanisms:
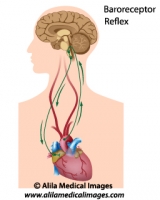
Pressure gradient: the difference between venous pressure and right atrial pressure is the major force driving peripheral blood back to the heart. In fact, venous return can be determined as the venous pressure gradient divided by venous resistance. Factors that increase venous pressure or decrease right atrial pressure, facilitate venous return. In principle, constriction of veins blocks blood flow, increases venous resistance and reduces venous return. However when blood vessels throughout the body are constricted, such as during sympathetic activation, the increased resistance causes blood pressure to rise, and this eventually overrides the increase in venous resistance. As a result, venous return increases.
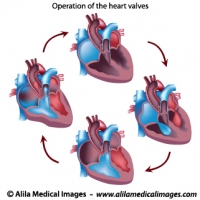
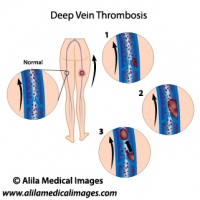
Skeletal muscle pump: Veins in the arms and legs are surrounded by skeletal muscles. They also have one-way valves in their walls that only open for upward flow. During everyday activities, such as walking, the muscles contract and squeeze blood in the veins upward, toward the heart. The one-way valves prevent blood from flowing down again when the muscles relax. This is one of mechanisms by which physical exercise increases cardiac output to meet the body’s needs.
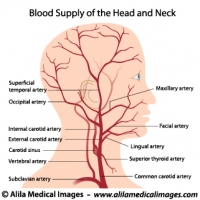
Gravity: In an upright position, venous blood from the head and neck flows downhill to the heart simply by gravity. Blood from the lower body and limbs, on the other hand, has to overcome gravity to return to the heart. People who stand or sit still for extended periods of time may suffer from venous blood pooling in the legs. This happens when venous pressure is not sufficient to override gravity and venous return is reduced. Because the heart cannot pump more blood than it receives, cardiac output may decrease, sometimes to a dangerous level, and the person may faint. One can prevent this from happening by activating the skeletal muscle pump, either by keeping the legs moving, or by tensing leg muscles periodically.
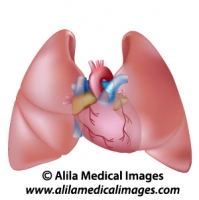
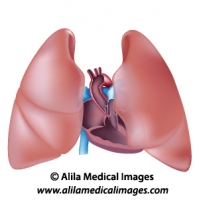
Breathing, or respiratory pump: during inspiration, the diaphragm moves down, expanding the thoracic cavity, resulting in a decreased intra-thoracic pressure and a subsequent expansion of the lungs. Part of this change in pressure is transmitted across the walls of the heart, lowering right atrial pressure and thus facilitating venous return. At the same time, the descent of the diaphragm also causes an increase in abdominal pressure. As the inferior vena cava passes through both abdominal and thoracic cavities, an increase in abdominal pressure together with a decrease in thoracic pressure squeeze the blood upward, toward the heart. Increasing the rate and depth of breathing is another way the body raises cardiac output during physical exercise.