Below is a narrated animation about glaucoma development and types of glaucoma. Click here to license this video and/or other eye and vision related videos on Alila Medical Media website.
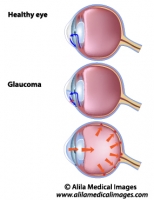
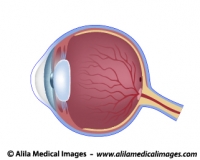
Glaucoma is a group of eye diseases in which the optic nerve is damaged leading to irreversible loss of vision. In most cases, this damage is due to an increased pressure within the eye – elevated intraocular pressure.
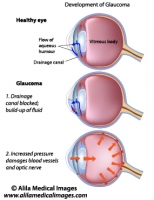
How glaucoma develops
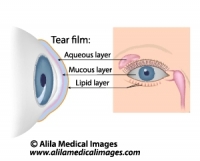
The eye produces a fluid called aqueous humor which is secreted by the ciliary body into the posterior chamber, a space between the iris and the lens. It then flows through the pupil into the anterior chamber between the iris and the cornea. From here, it is drained through a sponge-like structure located at the base of the iris called the trabecular meshwork and leaves the eye. In a healthy eye, the rate of secretion balances the rate of drainage.
In people with glaucoma, this drainage canal is partially or completely blocked. Fluid builds up in the chambers and this increases pressure within the eye. The pressure drives the lens back and presses on the vitreous body which in turn compresses and damages the blood vessels and nerve fibers running at the back of the eye. These damaged fibers result in patches of vision loss and if left untreated may lead to total blindness.
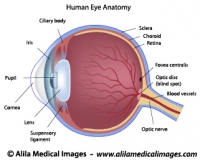
For eye anatomy basics click here.
Click here to see an animation of glaucoma progression on Alila Medical Media website where the video is also available for licensing.

Fig. 1 : Development of glaucoma. Click on image to see a larger version on Alila Medical Media website where the image is also available for licensing.
Open-Angle Glaucoma vs. Angle-Closure Glaucoma
These are the two main types of glaucoma. The “angle” here refers to the corner between the cornea and the iris where the trabecular meshwork is located.
Primary Open-Angle or Chronic Open-Angle Glaucoma is the most common form of glaucoma accounting for about 90% of cases. This is caused by partial blockage of the drainage canal. The angle is “open”, meaning the entrance to the drain is clear, but the flow of aqueous humor is somewhat slow. The pressure builds up gradually in the eye over a long period of time. There is no pain and visual loss appears gradually, starting from peripheral vision, and may go on unnoticed until the central vision is affected. Progression of glaucoma can be stopped with medical treatments, but part of vision that is already lost can not be restored. This is why it’s very important to detect signs of glaucoma early with regular eye exams.
Closed-angle or Acute angle-closure glaucoma (AACG) is less common. This type of glaucoma is caused by a sudden and complete blockage of aqueous humor drainage. The pressure within the eye rises rapidly and may lead to total vision loss quickly. This is a medical emergency and requires immediate attention. Symptoms to watch out for: sudden severe pain inside and around the eye, redness, blurry vision, seeing halos around a light, some people may also feel headache, nausea.
Certain anatomical features of the eye make it easier for AACG to happen. These include: narrow drainage angle, shallow anterior chamber, thin and droopy iris, lens sitting too much forward. These features are often inherited and so AACG incidents are likely to run in the family.

Fig. 2 : Open angle vs closed angle glaucoma. Click on image to see a larger version on Alila Medical Media website where the image is also available for licensing.
Typically, this is what happens in AACG : the pupil is dilated (e.g. when looking in the dark) and the lens is stick to the back of the iris. This prevents the aqueous humor from flowing through the pupil into the anterior chamber (primary block). As the fluid accumulates in the posterior chamber it presses on the iris causing it to bulge outward and block the drainage angle (secondary block).
Other types of Glaucoma
Normal pressure glaucoma – Some people can get glaucoma (vision loss due to damaged optic nerve) without elevated intraocular pressure. This may be due to poor blood supply (e.g. damaged blood vessels in diseases such as diabetes) to the nerve fibers.
Secondary glaucoma – glaucoma develops as a result of trauma after eye injuries.
Congenital glaucoma – glaucoma that is present at birth.
Treatments
Progression of glaucoma can be halted or slowed down with medical treatments, but part of vision that is already lost can not be recovered. This is why it’s very important to detect signs of glaucoma early with regular eye exams.
– Eye drops that lower intraocular pressure and/or reduce fluid production.
– Laser treatments : Laser is used to burn part of the trabecular meshwork to improve fluid flow – laser trabeculoplasty. It can also be used to remove part of the ciliary body to reduce fluid secretion. For acute glaucoma, small holes can be made in the iris to relieve the primary block – laser iridotomy.
– Eye surgeries: a procedure called trabeculectomy is used to create a channel – an alternative route – for aqueous fluid drainage. For acute glaucoma a procedure called iridectomy may be performed to drill a hole in the iris. Canaloplasty is a newer, less invasive surgical procedure performed for treatment of open angle glaucoma. This procedure involves enlargement of the eye’s natural drainage canal.
In people with AACG, laser and surgical treatments may be performed for the other, still healthy eye as well to prevent future development of glaucoma.